Predictive Analytics for Hospital Readmissions: Transforming Healthcare with Data
Posted by Komal Sharma
Filed in Health 256 views
Introduction
Hospital readmissions have long been a critical challenge in healthcare systems worldwide. Not only do they reflect the quality of care a patient receives, but they also contribute significantly to rising healthcare costs. According to the Centers for Medicare & Medicaid Services (CMS), nearly 20% of Medicare patients are readmitted within 30 days of discharge, resulting in billions of dollars in preventable expenses annually. As healthcare organizations strive to improve patient outcomes and reduce costs, predictive analytics has emerged as a transformative tool in tackling hospital readmissions.
Definition
Predictive Analytics for Hospital Readmissions refers to the use of data-driven models and statistical techniques to identify patients at high risk of being readmitted to the hospital after discharge. By analyzing clinical, demographic, and behavioral data, healthcare providers can anticipate potential complications, optimize care plans, and implement targeted interventions to reduce readmission rates, improve patient outcomes, and lower healthcare costs.
Understanding Hospital Readmissions
A hospital readmission occurs when a patient who was recently discharged returns to the hospital within a specified period, often 30 days, due to complications or insufficient recovery. Readmissions can result from multiple factors, including:
-
Inadequate discharge planning
-
Poor follow-up care
-
Medication errors
-
Chronic disease progression
-
Socioeconomic factors such as lack of access to proper nutrition or transportation
Frequent readmissions not only burden healthcare systems financially but can also negatively impact patient health, increase stress, and lower overall satisfaction with healthcare services. Reducing readmissions, therefore, has become a priority for hospitals aiming to improve both clinical outcomes and operational efficiency.
What is Predictive Analytics?
Predictive analytics is the use of historical data, statistical algorithms, and machine learning techniques to identify the likelihood of future outcomes. In the context of healthcare, it involves analyzing large datasets from electronic health records (EHRs), patient demographics, clinical notes, lab results, and social determinants of health to predict which patients are at higher risk of hospital readmission. Unlike traditional reactive approaches, predictive analytics allows healthcare providers to anticipate potential complications before they occur, enabling proactive interventions that can prevent unnecessary readmissions.
How Predictive Analytics Helps Reduce Readmissions
Risk Stratification:
Predictive models can segment patients based on their likelihood of readmission. By analyzing data points such as age, previous hospitalizations, chronic conditions, and medication adherence, healthcare providers can identify high-risk patients. For instance, a patient with congestive heart failure, diabetes, and poor post-discharge support may be flagged as high-risk, prompting additional follow-up care or monitoring.
Personalized Care Plans:
Once high-risk patients are identified, predictive analytics allows clinicians to tailor interventions to individual needs. This may include scheduling early follow-up appointments, providing home care services, or offering educational resources about managing chronic conditions. Personalized care plans improve patient engagement and adherence to treatment, significantly lowering the likelihood of readmission.
Improved Discharge Planning:
Effective discharge planning is critical to preventing readmissions. Predictive analytics can highlight patients who may struggle after discharge due to social, medical, or behavioral challenges. Hospitals can then implement strategies such as arranging transportation, coordinating with primary care providers, or enrolling patients in post-discharge programs.
Resource Optimization:
By predicting which patients are most likely to be readmitted, hospitals can allocate resources more efficiently. High-risk patients may receive more intensive follow-up care, while low-risk patients may require minimal intervention. This targeted approach ensures optimal use of staff, time, and financial resources.
Monitoring and Early Intervention:
Some predictive analytics tools use real-time data from wearable devices and remote monitoring systems to track patients’ vital signs and health metrics after discharge. Early detection of concerning trends, such as elevated blood pressure or fluctuating glucose levels, can trigger immediate interventions, preventing hospital readmissions.
Key Data Sources for Predictive Analytics
Predictive analytics relies on diverse datasets to generate accurate insights. Common data sources include:
-
Electronic Health Records (EHRs): Contain patient demographics, medical history, lab results, medications, and clinical notes.
-
Claims Data: Provides information on previous hospital visits, treatments, and billing codes.
-
Social Determinants of Health (SDOH): Includes data on socioeconomic status, living conditions, and access to care.
-
Patient-Reported Outcomes: Surveys and feedback regarding patient well-being, medication adherence, and post-discharge challenges.
-
Wearable Devices and Remote Monitoring Tools: Track vital signs, activity levels, and chronic disease management metrics in real-time.
Integrating these data sources into predictive models enhances the accuracy of readmission risk predictions, allowing healthcare providers to make informed decisions.
Machine Learning in Predictive Analytics
Machine learning algorithms are at the heart of predictive analytics for hospital readmissions. These algorithms can detect patterns and relationships in complex datasets that may not be apparent to human analysts. Common approaches include:
-
Logistic Regression: Often used to predict the probability of readmission based on multiple patient characteristics.
-
Decision Trees and Random Forests: Analyze combinations of variables to classify patients as high or low risk.
-
Neural Networks: Capable of identifying complex, non-linear relationships between multiple factors contributing to readmissions.
-
Gradient Boosting Machines (GBM): Build robust models by iteratively improving prediction accuracy.
Hospitals can deploy these models to generate risk scores for each patient, guiding clinical decision-making and intervention planning.
Benefits of Predictive Analytics in Reducing Readmissions
-
Enhanced Patient Outcomes: Early identification of high-risk patients allows for timely interventions, reducing complications and improving recovery rates.
-
Cost Savings: Preventing avoidable readmissions reduces healthcare expenses for both hospitals and patients.
-
Regulatory Compliance: In many regions, hospitals face penalties for excessive readmissions. Predictive analytics helps institutions meet quality standards and avoid financial penalties.
-
Operational Efficiency: Data-driven insights help hospitals allocate resources effectively, streamline workflows, and improve overall efficiency.
-
Patient Engagement: Personalized care and proactive follow-up foster stronger patient-provider relationships, improving adherence to treatment plans.
Challenges and Considerations
While predictive analytics holds tremendous promise, implementing it effectively requires addressing several challenges:
-
Data Quality and Integration: Incomplete or inconsistent data can undermine model accuracy. Integrating data from disparate sources remains a significant hurdle.
-
Privacy and Security: Patient data must be protected under regulations like HIPAA. Ensuring secure data storage and processing is critical.
-
Model Transparency: Clinicians must understand how predictive models make decisions to trust and act on their recommendations.
-
Bias and Equity: Predictive models must be carefully designed to avoid perpetuating biases based on race, gender, or socioeconomic status.
Addressing these challenges requires a combination of robust technology, skilled data scientists, and clinical expertise.
Future Trends of Predictive Analytics for Hospital Readmissions Market
AI and Machine Learning Advancements:
The adoption of advanced AI and machine learning algorithms is expected to grow, enabling more accurate predictions of hospital readmissions. Models will become increasingly capable of analyzing complex patient data, including real-time monitoring and unstructured clinical notes.
Integration of Social Determinants of Health:
Future predictive analytics solutions will increasingly incorporate social determinants of health - such as socioeconomic status, living conditions, and access to care - allowing hospitals to address broader factors influencing readmission risks.
Real-Time Remote Monitoring:
Wearable devices and telehealth solutions will facilitate continuous patient monitoring after discharge. Predictive analytics platforms will leverage this data to detect early warning signs, prompting timely interventions that prevent avoidable readmissions.
Personalized Patient Care:
Predictive insights will drive highly personalized care plans, tailoring interventions for each patient based on risk profiles. This approach enhances patient engagement, adherence, and overall recovery outcomes.
Market Growth and Adoption:
The hospital readmission predictive analytics market is poised for significant growth, driven by regulatory pressures, cost-saving initiatives, and the rising focus on value-based healthcare. Hospitals worldwide are expected to increasingly invest in data-driven solutions to improve outcomes and operational efficiency.
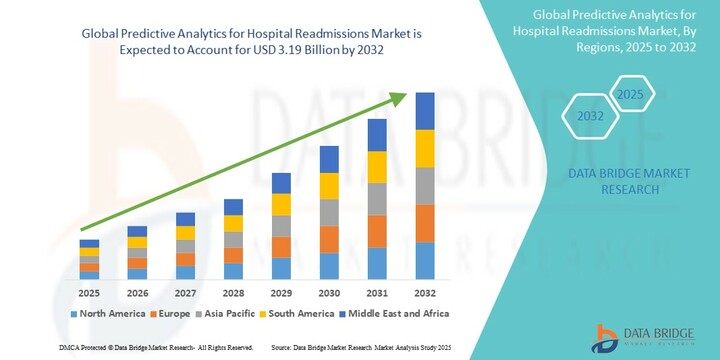
Growth Rate of Predictive Analytics for Hospital Readmissions Market
According to Data Bridge Market Research, the size of the global predictive analytics for hospital readmissions market was estimated at USD 1.18 billion in 2024 and is projected to grow at a compound annual growth rate (CAGR) of 13.30% to reach USD 3.19 billion by 2032.
Conclusion
Hospital readmissions pose a significant challenge to healthcare systems, but predictive analytics offers a powerful solution. By leveraging historical data, machine learning, and real-time monitoring, hospitals can identify high-risk patients, implement personalized care plans, and prevent avoidable readmissions. The benefits are clear: improved patient outcomes, cost savings, enhanced operational efficiency, and better regulatory compliance.